-
Evaluation
A detail interview is performed in order to decide the best treatment modality for the couple. Past examination and treatment documentations are reviewed. A pelvic exam is performed for the woman and a specimen is obtained for smear test and bacteriologic examination, if required. Uterus and ovaries are examined with ultrasonography. The hormone profile analyzed in Day 3 of the period helps the treatment plan. A histerosalpingography can be ordered, if required. Semen analysis is ordered for the man. Considering relevant conditions of the couple and review of the results, the treatment protocol and the dose of the medication are decided.
-
Ovulation Induction
A healthy woman releases 1 or 2 eggs from the ovaries. Considering in vitro fertilization therapy, the aim is to promote release of many eggs (oocytes). At this stage, folic acid supplement is started to prevent any abnormality in the fetal nervous system. The treatment is initiated with the pre-determined protocol and the dose. Patients are asked to present for ultrasonographic evaluation at certain intervals in order to evaluate number and diameter of follicles. The aim is to obtain 10 to 12 follicles, each measuring 16 to 20 mm in size. Hormone analyses may be ordered during the follow-up in order to adjust dose of the drug. In follow-up visits, endometrium – the interior lining of the uterus – is also evaluated with ultrasonography. Induction of ovulation and maturation of egg takes 10 to 12 days. Women should be checked every day or every other day through the end of the treatment. After follicles reach a certain size, hCG is administered to ensure the final maturation. Oocytes are picked up approximately 36 hours after the hCG injection.
-
Oocyte Pick Up
The couple should necessarily visit the in vitro fertilization center at the scheduled date and time. The patient should not eat and drink after 00:00 the night before the procedure day. Oocyte pick up is usually performed in the operating theater under general anesthesia and the procedure lasts approximately 15 to 20 minutes. The patient is placed on gynecologic table and a special needle is inserted and advanced to ovaries under guidance of transvaginal ultrasound. Each follicle is punctured and intrafollicular fluid is emptied with vacuum. The fluid is immediately transferred to the embryology laboratory and it is examined by embryologists under microscope. Eggs are sorted in the fluid and they are collected in another container filled with culture medium; the number is determined and they are stored in special cabinets, called incubator that creates an environment similar to the mother’s womb, until they are fertilized. Thus, all follicles are aspirated and the procedure is ended. Number of picked up oocytes may differ from the number of follicles visualized in ultrasound scan in the follow-up; here, the matter is the number of oocytes we have. The patient is recovered from anesthesia and transferred to the room after the procedure. The patient is allowed to rest after the procedure and discharged to home following information about number of oocytes picked up and instructions about medications, if all controls are normal and the patient feels well. A pain similar to menstrual pain may be felt in groins for 2 to 3 days. It can be managed with painkillers. Leakage or mild drop-like bleeding can persist for several days.
-
Fertilization
Two methods are available for this purpose:
Conventional In Vitro Fertilization (IVF):
It is mostly preferred for group of young couples characterized by abundant oocytes and good sperm characteristics. The follicular fluid transferred to the embryology laboratory in sterile tubes is examined by an embryologist under microscope in a special cabin and the oocytes are transferred into a special medium. Eggs are allowed to stay with sperms in containers specially prepared for the procedure (100 thousand to 200 thousand mobile sperms for each egg) for 16 to 18 hours in order to ensure that the sperm fertilizes the egg without any manipulation. Fertilization is checked at the end of this period. Even if IVF is decided, microinjection can be performed for a part of eggs in order to rule out the risk of a fertilization failure.
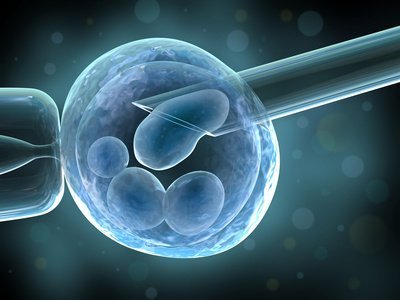
Microinjection – ICSI (Intracytoplasmic Sperm Injection)
Microinjection is preferred for following cases: sperms characterized by low count and mobility and significant deformity; inability to obtain sperm with surgical techniques (TESA, TESE); oocytes picked up from the woman are poor in number and/or quality; oocyte membrane is too thick; the diagnosis is idiopathic infertility; and the couple has past history of unsuccessful IVF attempts. Retrieved eggs are sorted and liberated from the cell residues (cumulus cells) and finally, the mature eggs are selected. Fertilization is performed approximately 2 to 6 hours after the eggs are retrieved. Sperm is injected into the egg by the embryologist who uses a special device, called micromanipulator, under microscope. They are left in the incubator and the fertilization is checked 16 to 18 hours afterwards. Today, microinjection (ICSI) method, which increases the rate of fertilization, is performed instead of IVF in assisted reproductive therapies. Since only one single sperm cell is sufficient for fertilization of an egg through natural means, microinjection allows men with very low sperm count be a father. Approximately 70% of the retrieved eggs are mature and appropriate for fertilization. Approximately 70 of them will be fertilized. For example, a woman with 10 eggs has 7 to 8 mature eggs on average, resulting in 4 to 5 embryos. This is an average figure and the actual number may be higher or lower.