What is atherosclerosis?
Atherosclerosis, commonly known as atherosclerosis, is one of the leading causes of heart disease and stroke. Worldwide, atherosclerosis and its complications are the leading cause of death. The hardening that develops when substances accumulate in the arteries and form plaques can completely block the arteries over time and cause serious problems in the body. A good understanding of the factors that lead to this disease, which usually develops with aging, is essential for the prevention and treatment of the disease.
What is Atherosclerosis?
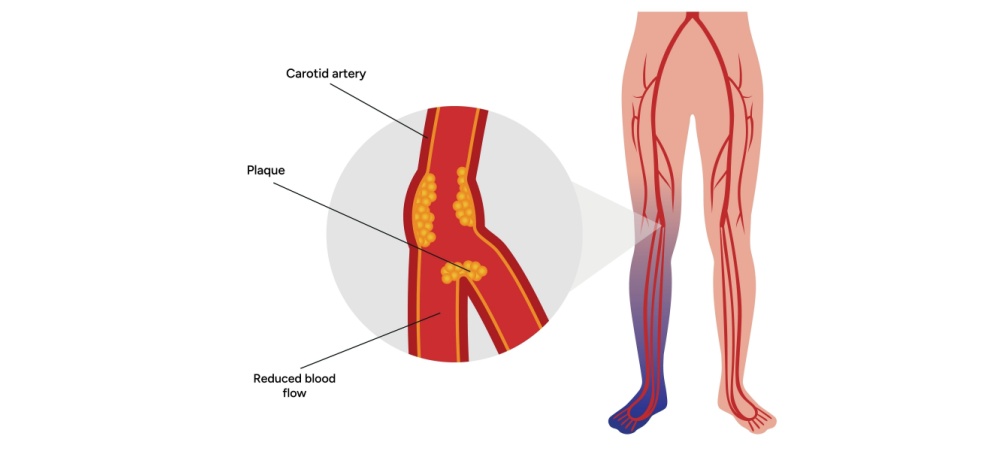
Atherosclerosis is a cardiovascular disease caused by plaque in the arteries, which is a buildup of cholesterol, fat, blood cells, cellular waste, fibrin, calcium and other substances found in the blood. This plaque is a sticky substance that hardens over time, causing the arteries to narrow. This limits the flow of oxygen-rich blood through the body and causes many complications. Atherosclerosis is a slow, progressive disease that can start in childhood and worsens with age, although there are cases of rapid progression. Although the causes of atherosclerosis are not fully understood, it is thought that unhealthy lifestyle habits, the presence of other diseases and genetic predisposition can lead to damage. Most arteries in the body can be affected by plaque formation. Depending on which artery it affects, it can have different names:
- Coronary Artery Disease: Develops due to plaque build-up in the arteries of the heart.
- Peripheral Artery Disease: Develops due to plaque formation in the arteries that carry blood from the heart to the body. It can affect the arteries of the legs, arms and pelvis.
- Carotid artery disease: Plaque builds up in the artery in the neck and reduces blood flow to the brain.
- Renal Artery Stenosis: Plaque buildup in the arteries that supply blood to the kidneys.
- Vertebral Artery Disease: Plaque buildup in the arteries that provide blood flow to the back of the brain.
- Mesenteric Artery Ischemia: It is a condition in which the arteries that supply blood to the intestines cannot provide adequate blood flow due to plaque formation.
What are the Symptoms of Atherosclerosis?
Atherosclerosis usually does not cause any symptoms in the early stages. Some patients do not show any symptoms until their arteries are completely blocked and they have a heart attack or stroke. Symptoms begin to develop when the body’s oxygen demand increases and different symptoms may develop depending on which artery is narrowed:
- Unusual heartbeat and arrhythmia,
- Heart palpitations
- Pain or pressure in the upper body, such as the chest, arms, neck and jaw (this condition is commonly known as angina),
- Difficulty breathing, shortness of breath.
Symptoms of cerebral arteriosclerosis include:
- Numbness or loss of strength in the arms or legs,
- Speaking, thinking and comprehension difficulties,
- Contraction of the facial muscles,
- Transient ischemic attacks,
- Paralysis
- Severe headache,
- Problems with vision in one or both eyes.
Symptoms of atherosclerosis in the arms, pelvis and feet:
- Intermittent claudication, i.e. leg pain when walking,
- Numbness,
- Cold feet,
- Pain or burning in the toes and feet during rest,
- Frequent non-healing sores and infections of the feet.
Symptoms related to the kidneys are as follows:
- High blood pressure (hypertension),
- Kidney failure.
Symptoms of atherosclerosis developing in the vessels affecting the intestine are as follows:
- Extreme pain after meals,
- Weight loss,
- Diarrhea
Other symptoms are briefly as follows:
- Erectile dysfunction for men,
- Blood clots and serious complications due to clots.
What are the Risk Factors for Atherosclerosis?
Atherosclerosis is a serious medical condition categorized as cardiovascular disease. It is a slow progressive disease that starts at a young age. According to studies, if a person is 40 years old and in good general health, there is a 50% chance of developing severe atherosclerosis [1]. The risk of the disease increases with age. Adults over 60 years of age usually have some atherosclerosis, but may not have severe symptoms. Atherosclerosis risk factors increase the likelihood of developing the disease. Up to 90% of heart attacks are caused by these risk factors [1]:
- Obesity
- Diabetes and insulin resistance,
- Family history of cardiovascular disease,
- Excessive alcohol consumption,
- High blood pressure,
- High LDL cholesterol,
- High levels of the inflammatory signal known as C-reactive protein in the blood,
- High triglyceride levels,
- Unhealthy eating habits, lack of fruit and vegetable consumption,
- Insufficient physical activity,
- Sleep apnea
- Metabolic syndrome
- Inflammatory diseases such as rheumatoid arthritis and psoriasis,
- Smoking or chewing tobacco,
How is Atherosclerosis Diagnosed?
When diagnosing atherosclerosis, physicians start with a physical examination. They ask various questions to learn about patients’ symptoms. The patient’s medical and family health history is obtained, and questions are asked about lifestyle and risk factors for plaque formation in the arteries. A number of tests may be ordered based on the symptoms shown, the answers to the questions posed to the patient and the physical examination:
- Blood Tests: Blood tests are usually performed to monitor blood sugar and cholesterol levels. High levels of blood sugar or cholesterol can lead to an increased risk of atherosclerosis. Blood tests may also be performed to detect levels of CRP, a protein linked to inflammation of the arteries.
- Electrocardiography (ECG): A quick and painless test that measures the electrical activity of the heart. During an ECG, electrodes are attached to the chest and, if necessary, to the arms and legs. It is a procedure that allows changes in the amount of blood flow to the heart to be understood.
- Echocardiography: A diagnostic test that uses sound waves to show blood flow in the heart. In some cases, it can be performed in combination with an exercise stress test.
- Exercise Stress Test: Physicians may order this test if symptoms usually occur during exercise or physical activity. The heart is monitored while the patient walks or runs on a treadmill. The heart pumps harder and faster during exercise than during daily activities. An exercise stress test can therefore help diagnose heart problems that might otherwise be missed. If there is a condition that prevents exercise, the patient may be given medication that mimics the effect of exercise on the heart.
- Doppler Ultrasound: Doppler ultrasound can be used to measure blood pressure at various points on the arm or leg. During this measurement, the blood flow rate in the arteries can be detected.
- Ankle-Arm Index (ABI): Allows comparison of blood pressure in the ankle and arm, diagnosing narrowed arteries and weakened blood flow. It is a quick and simple way to detect peripheral arterial disease caused by atherosclerosis.
- Cardiac Catheterization and Angiography: It helps to diagnose whether the coronary arteries are narrowed or blocked. A thin and flexible tube, called a catheter, is inserted into the appropriate blood vessels and advanced towards the heart. Dye flows through the catheter into the heart artery and makes the images taken during the test clearer.
- Coronary Calcium Scan: Also known as a heart scan. Computed tomography is used to obtain detailed pictures of the heart. Images of calcium deposits in the artery wall are obtained. The test results are scored in points. When calcium is present, the score is high, and a high score means a high risk of heart disease.
How is atherosclerosis treated?
Once a plaque has formed, it usually stays there. With procedures such as medical treatment procedures and changes in living habits, the formation of plaques can be slowed or stopped. Some atherosclerosis treatment procedures can even shrink plaques. The following information can be given about atherosclerosis treatment methods:
- Lifestyle Changes: Atherosclerosis can be slowed down by paying attention to risk factors. Some changes such as healthy eating habits, physical activity and not smoking can be implemented. Although these changes do not eliminate blockages, they reduce the risk of heart attack and stroke.
- Medicines: Medicines for high cholesterol and blood pressure can slow down atherosclerosis. They can lower low-density lipoprotein (LDL) cholesterol, thin the blood, prevent blood clots and control health conditions such as diabetes.
- Angiography and stenting: A thin tube is inserted into arteries in the leg and arm to reach the diseased artery. Blockages can be seen vividly on an X-ray screen. Angioplasty and stenting can open blocked arteries and relieve symptoms.
- Bypass Surgery: A treatment procedure in which healthy blood vessels in the leg or chest are removed and used instead of the blocked vessel. It basically aims to create a new pathway for blood.
- Endarterectomy: A procedure in which the plaque is removed and blood flow is restored. If the procedure is performed on the carotid artery in case of arteriosclerosis in the neck, it is called carotid endarterectomy. Stents may also be placed in high-risk patients.
- Fibrinolytic Therapy: If there is a clot blocking the arteries, clot-dissolving medicines are administered.
Frequently Asked Questions About Atherosclerosis
Are Arteriosclerosis and Vascular Occlusion the Same Thing?
Arteriosclerosis and atherosclerosis are not the same thing. Arteriosclerosis is the thickening of the arterial wall due to the accumulation of substances such as fat, forming plaque and hardening of this plaque. When these deposits increase and obstruct blood flow, it can lead to atherosclerosis. In other words, arteriosclerosis and arteriosclerosis are different conditions, arteriosclerosis can lead to arteriosclerosis over time.
Which Doctor to Go to for Arteriosclerosis?
The cardiology department can be consulted for the diagnosis and treatment of atherosclerosis. Atherosclerosis is a cardiovascular disease and physicians who specialize in these diseases are called cardiologists. It is the duty of cardiologists to diagnose atherosclerosis, create a treatment plan and monitor the process. Cardiologists may also receive support from dieticians and physical therapists if they deem it necessary. They can also refer to cardiovascular surgeons in case a surgical intervention is necessary.
Who Has Atherosclerosis?
People with a family history of high blood cholesterol, hypertension, diabetes, inflammatory diseases and people over the age of 45 in men and 55 in women may develop atherosclerosis. In addition, atherosclerosis can also be seen in people with high saturated fat consumption, smoking and drinking alcohol.
Does Stress Cause Atherosclerosis?
Stress can negatively affect many physiological processes in the body, disrupt hormone balance and cause negative pathological conditions on blood vessels. Therefore, it is especially necessary for patients with atherosclerosis to find ways to help reduce emotional stress. This can include exercise, psychological counseling, yoga and deep breathing exercises.
What to Do to Avoid Atherosclerosis?
To prevent atherosclerosis, lifestyle changes are recommended. It is necessary to quit smoking, adopt healthy dietary habits, engage in regular physical activity and maintain a healthy weight. In addition, regular checks of blood pressure, cholesterol and blood sugar levels are also among the measures that can be taken.
What Negativities Does Arteriosclerosis Cause?
Atherosclerosis can lead to different complications depending on which artery it develops in. Atherosclerosis can cause coronary artery disease, carotid artery disease, peripheral artery disease, aneurysms and chronic kidney disease.